Introduction
Physiotherapy in Kitchener for Lower Back
Welcome to Kitchener Physiotherapy & Wellness patient resource about Lumbar Spondylolysis.
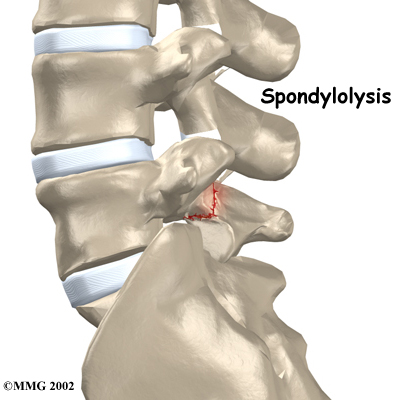
Spondylolysis happens when a crack forms in the bony ring on the back of the spinal column. Most commonly, this occurs in the low back. In this condition, the bone that protects the spinal cord fractures as a result of excessive or repeated strain. The area affected is called the pars interarticularis, so doctors sometimes refer to this condition as a pars defect.
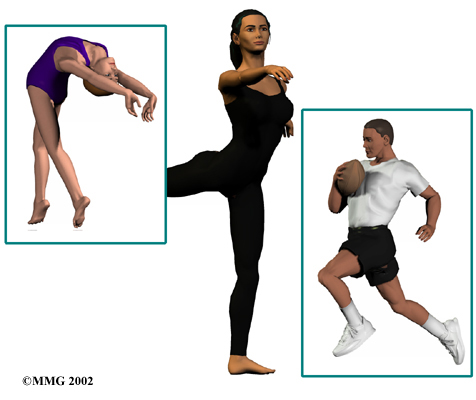
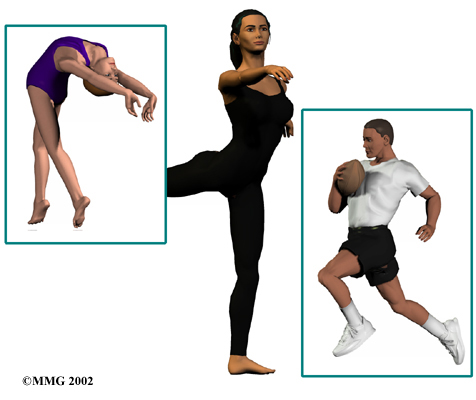
This condition appears in six percent of children. It mainly affects young athletes who participate in sports in which the spine is repeatedly bent backwards, such as gymnastics, football, and karate.
Although spondylolysis can affect people of any age, children and adolescents are most susceptible. This is because their spines are still developing, and the pars is the weakest part of the vertebra. Placing extra strain on this area of the spine during childhood increases the chance that a pars defect will occur.
This article will help you understand:
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the spine are involved?
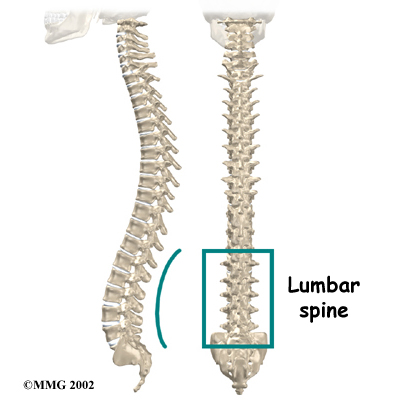
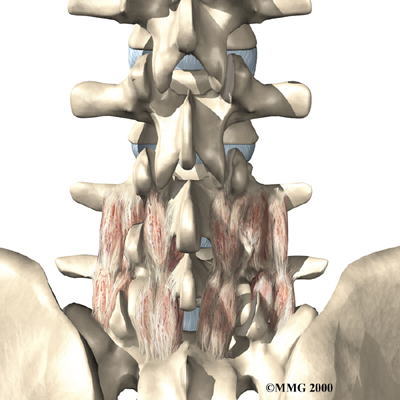
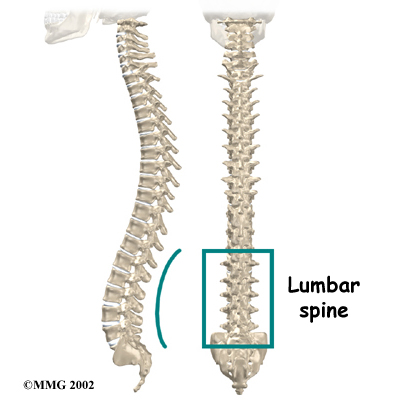
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to create the . The spinal column gives the body its form. It is the body's main upright support. The section of spine in the lower back is called the lumbar spine.
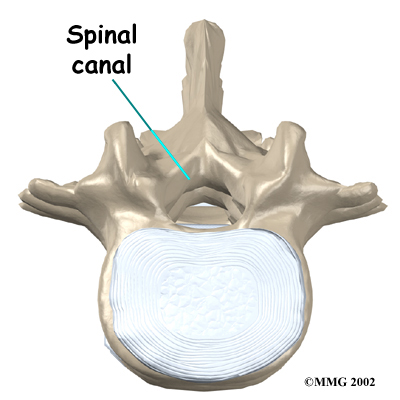
Each vertebra is formed by a round block of bone, called a vertebral body. A circle of bone attaches to the back of the vertebra. When the vertebrae are stacked on top of each other, these bony rings create a hollow tube. This tube, called the , surrounds the spinal cord as it passes through the spine. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
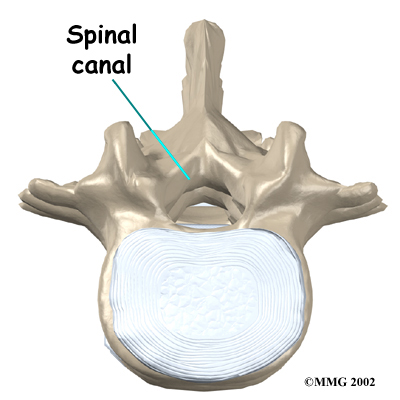
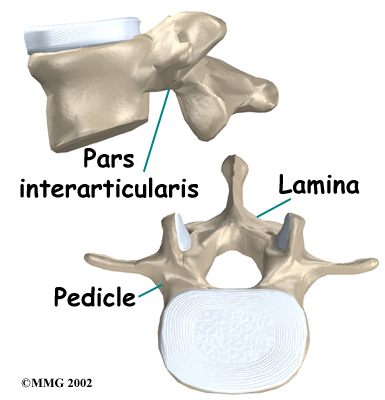
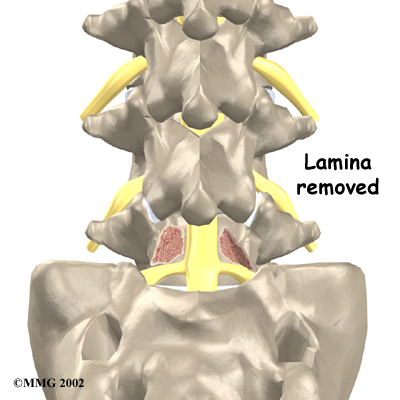
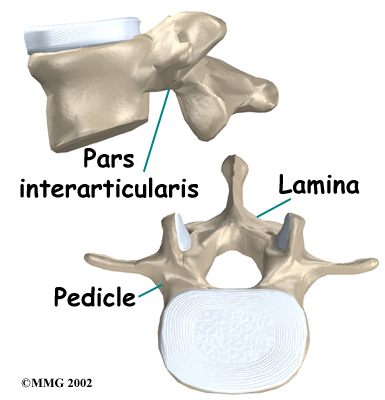
The protective ring that surrounds the spinal cord is a continuous ring of bone. Its sections include two pedicles, which attach directly to the back of the vertebral body. Two laminae complete the ring.
The pedicles and laminae are two different areas of the bony ring. The area between them is not a joint. Rather, it is a location in the continuous ring of bone that doctors call the pars interarticularis, or pars for short. There are two such meeting points on the back of each vertebra, one on the left and one on the right. The pars is thought to be the weakest part of the .
Related Document: Kitchener Physiotherapy & Wellness Guide to Lumbar Spine Anatomy
Causes
What causes this problem?
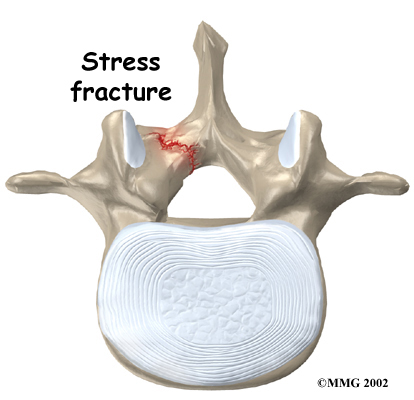 Spondylolysis is thought to be caused by repeated strains that damage the lower spine over time. The repeated strains can eventually lead to an overuse injury in the pars interarticularis. The most common location for this to occur is in the lowest vertebra of the spine, which doctors call L5. This vertebra connects the spine to the pelvis. However, a problem with the pars can occur in any lumbar vertebra. It rarely happens in more than one vertebra at a time.
Spondylolysis is thought to be caused by repeated strains that damage the lower spine over time. The repeated strains can eventually lead to an overuse injury in the pars interarticularis. The most common location for this to occur is in the lowest vertebra of the spine, which doctors call L5. This vertebra connects the spine to the pelvis. However, a problem with the pars can occur in any lumbar vertebra. It rarely happens in more than one vertebra at a time.
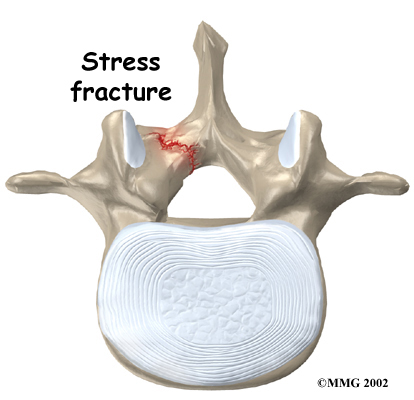
The vertebra initially responds to the abnormal strain by adding new bone cells around the injured area. But if the injuries happen faster than the body can keep up with needed repairs, a crack may form in the weakened bone. This is called a . This type of fracture occurs in the pars, the area of bony ring between the pedicle and lamina.
The crack may affect only one side of the bony ring. However, it is equally common for the defect to occur on both sides. When this happens, the vertebra is no longer held firmly in place by the facet joints on the back of the ring. As a result, the vertebra is free to slip forward over the one below. This slippage, which is closely related to spondylolysis, is called .
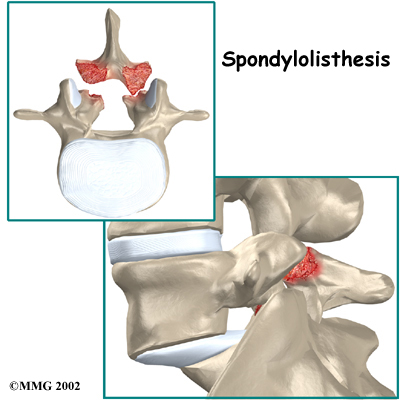
Related Document: Kitchener Physiotherapy & Wellness Guide to Spondylolisthesis
Spondylolysis commonly occurs in young gymnasts who regularly practice as part of their routines. Football linemen and dancers are also prone to spondylolysis. Symptoms sometimes appear when an athlete quickly ramps up his or her training intensity, applies incorrect technique, or uses poor equipment.
Symptoms
What does the condition feel like?
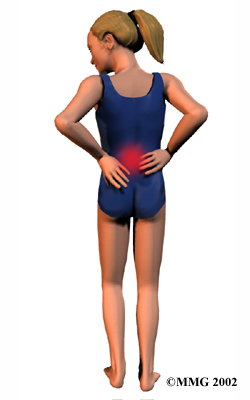
People with spondylolysis may feel pain and stiffness in the center of the low back. Bending fully backward increases pain. Symptoms typically get worse with activity and go away with rest. Doctors refer to this type of back pain as mechanical pain because it most likely comes from excess movement between the vertebrae.
 Individuals may eventually experience pain that radiates down one or both legs. This pain may come from pressure and irritation on the nerves that exit the spinal canal near the fracture. When nerve pressure in the low back causes leg pain, doctors refer it as neurogenic pain.
Individuals may eventually experience pain that radiates down one or both legs. This pain may come from pressure and irritation on the nerves that exit the spinal canal near the fracture. When nerve pressure in the low back causes leg pain, doctors refer it as neurogenic pain.
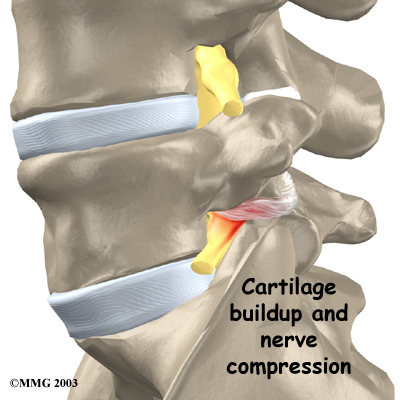
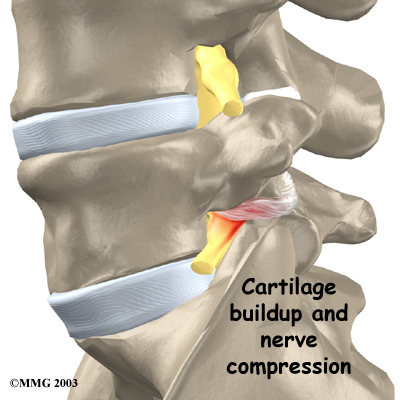
The cause of this nerve pressure is a result of the body's attempt to heal the stress fracture. Over time, the healing process may cause a bump of extra cartilage to grow at the site where the bones are trying to heal the overuse injury. If builds up, this bump may intrude into the opening where the nerves exit the spine. The bump may squeeze the nerve. This can produce pain and weakness in the leg. Reflexes become slowed. The person may also notice a pins and needles sensation in the skin where the spinal nerve travels.
Diagnosis
How do health care providers diagnose the problem?
Diagnosis begins with a complete history and physical exam. When you visit Kitchener Physiotherapy & Wellness, we will ask questions about your symptoms and how the problem is affecting your daily activities. You will be asked about your involvement in sports and your level of performance, as spondylolysis is a problem seen more often in football linemen, gymnasts, and those in similar sports that require intensive levels of performance. Our physiotherapist will also want to know what positions or activities make your symptoms worse or better.
Next our physiotherapist will examine you by checking your posture and the amount of movement in your low back. We check to see which back movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are also tested.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physiotherapists at Kitchener Physiotherapy & Wellness have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Our Treatment
Non-surgical Rehabilitation
After evaluating your condition, your physiotherapist at Kitchener Physiotherapy & Wellness my initially suggest that you rest your back by limiting your activities. The purpose of this is to help decrease inflammation and calm muscle spasm. You may need to take some time away from your sport, especially if it requires repeated back bending. This gives your back a chance to heal. Most patients who follow these measures get better. Only in severe cases are our patients counseled to completely discontinue participating in their sport.
Once you have rested your back to allow it to heal, we can develop a personalized physiotherapy program to help you fully recover. Although recovery time varies among individuals, as a guideline, you can expect to work with our physiotherapist a few times each week for four to six weeks. In severe cases, patients may need a few additional weeks of physiotherapy.
The first goal of treatment is to control symptoms. Your physiotherapist works with you to find positions and movements that ease pain. Treatments of heat, cold, ultrasound, and electrical stimulation may be used to calm pain and muscle spasm.
We will assign positions and exercises to ease your symptoms. Our physiotherapist will design an exercise program to improve the strength and control of your back and abdominal muscles. By watching you perform your sport activity, our physiotherapist can suggest style, technique, or equipment changes to improve your performance and prevent future problems.
As you recover, you will gradually advance in a series of strengthening exercises for the abdominal and low back muscles. Working these core muscles helps patients begin moving easier and lessens the chances of future pain and problems.
When needed, the physiotherapists at Kitchener Physiotherapy & Wellness can work closely with a sports coach on strategies for a patient's safe return to his or her sport. The two may provide suggestions on technique, equipment, and training frequency and intensity.
Most adolescents get better after wearing a brace or cast for a few months. Even then, a CT scan sometimes shows an unhealed fracture. In these cases, however, symptoms often go away completely, allowing a safe return to sports. Patients do best when guided in a gradual manner with the supervision of a therapist and sports coach.
If you are a working adult, our physiotherapist may also work with your doctor and employer to help you get back on the job as quickly as reasonably possible. You may be required to do lighter duties at first and progress to normal work activities. Our physiotherapist may also suggest changes that could help the patient work safely, with less chance of re-injuring his or her back.
A primary purpose of physiotherapy is to help patients learn how to take care of their symptoms and prevent future problems. Kitchener Physiotherapy & Wellness patients are given a home program of exercises to continue to improve flexibility, posture, endurance, and low back and abdominal strength. Our physiotherapist will also describe strategies you can use if your symptoms flare up.
Post-surgical Rehabilitation
Rehabilitation after surgery is more complex. Some patients leave the hospital shortly after surgery. However, some surgeries require patients to stay in the hospital for a few days. Although recovery time varies, patients who've had lumbar fusion surgery normally need to wait at least six weeks before beginning a rehabilitation program. This delay gives the fusion a chance to start healing. As a guideline, patients typically need to attend physiotherapy sessions for six to eight weeks and should expect full recovery to take up to six months.
At Kitchener Physiotherapy & Wellness, our goal is to help speed your recovery so that you can more quickly return to your everyday activities. When your recovery is well under way, regular visits to our office will end. We will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Kitchener Physiotherapy & Wellness provides services for physiotherapy in Kitchener.
Physician Review
Doctors often begin by prescribing nonsurgical treatment for spondylolysis. This is because symptoms from these stress fractures often resolve with rest or bracing. In some cases, doctors simply monitor their patients' condition to see if symptoms improve.
Your doctor may order an X-ray of your low back. An angled, or oblique, view is often used to check for a pars fracture. The doctor traces around the vertebral body and bony ring on the X-ray film. The outline normally forms an image that looks like a small dog. When a crack is present, however, the dog will appear to have a collar around its neck. This is referred to as the Scotty dog sign. It confirms a diagnosis of spondylolysis. An X-ray may be taken every few months to check how well the area is healing.
Small defects in the bone may not show up on X-ray. Also, a recent stress fracture won't always appear on X-ray. As a result, your doctor may order a bone scan to get the most accurate information. This involves injecting chemical "tracers" into your blood stream. The tracers then show up on special spine X-rays. The tracers collect in areas of extra stress to bone tissue, such as a stress fracture of the pars interarticularis.
Computed tomography (a CT scan) may be ordered. This is a detailed X-ray that lets doctors see slices of the body's tissue. The image can show if the edges of the fractured bone have begun growing together. The scan shows whether the fracture is new or old, so doctors can decide which treatments will help the most.
When more information is needed, your doctor may order a magnetic resonance imaging (MRI) scan. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. It can help in the diagnosis of spondylolysis. It can also provide information about the health of nearby intervertebral discs and other soft tissues that don't appear on X-rays.
If the doctor feels that the problem is due to a recent fracture, you may be placed in a rigid back brace or cast for three to four months. Keeping the spine from moving can help ease pain and inflammation. It can also improve the chances the bones will grow back together. Most people who require a brace or cast overcome symptoms and are able to eventually get back to activities free of pain. This can happen even when follow-up tests show that the bones haven't completely healed.
Once you have rested your back to allow it to heal, your doctor may recommend that you work with a physiotherapist a few times each week for four to six weeks. In severe cases, patients may need a few additional weeks of physiotherapy.
Surgery
 Most patients with spondylolysis do not require surgery. When symptoms are not relieved with nonsurgical treatments, however, patients may require surgery. The main types of surgery for spondylolysis include
Most patients with spondylolysis do not require surgery. When symptoms are not relieved with nonsurgical treatments, however, patients may require surgery. The main types of surgery for spondylolysis include
- laminectomy
- posterior lumbar fusion
Laminectomy
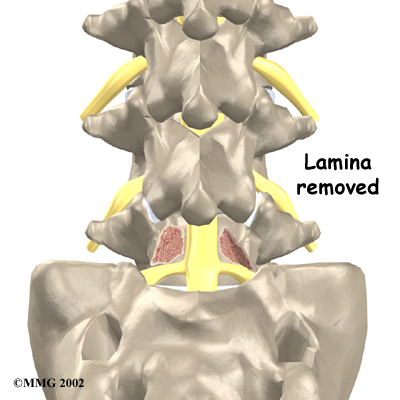
Nerve compression can cause considerable pain and symptoms. If too much cartilage builds up where the fractured bones are trying to heal, the nerve that passes near the injured bone may get squeezed, as described earlier. To fix this, a section of the bony ring is removed to take pressure off the nerve. The procedure to remove the lamina from the bony ring and release pressure on the nerve is called .
Related Document: Kitchener Physiotherapy & Wellness Guide to Lumbar Laminectomy
Posterior Lumbar Fusion
 A spinal fusion may be required after a surgeon performs a laminectomy procedure. Fusion is recommended when a spinal segment (a set of vertebrae) has become too loose or unstable.
A spinal fusion may be required after a surgeon performs a laminectomy procedure. Fusion is recommended when a spinal segment (a set of vertebrae) has become too loose or unstable.
A allows two or more bones to grow together, or fuse, into one solid bone. This keeps the bones and joints from moving. In this procedure, the surgeon lays small grafts of bone over the problem area on the back of the spine. Some surgeons also apply metal plates and screws to prevent the two vertebrae from moving. However, this practice is controversial because fusion occurs in about 90 percent of children with spondylolysis when the procedure is done without plates and screws.
Related Document: Kitchener Physiotherapy & Wellness Guide to Posterior Lumbar Fusion
During recovery from surgery, patients should follow their surgeon's instructions about wearing a back brace or support belt. They should be cautious about overdoing activities in the first few weeks after surgery.
Portions of this document copyright MMG, LLC.









 Spondylolysis is thought to be caused by repeated strains that damage the lower spine over time. The repeated strains can eventually lead to an overuse injury in the pars interarticularis. The most common location for this to occur is in the lowest vertebra of the spine, which doctors call L5. This vertebra connects the spine to the pelvis. However, a problem with the pars can occur in any lumbar vertebra. It rarely happens in more than one vertebra at a time.
Spondylolysis is thought to be caused by repeated strains that damage the lower spine over time. The repeated strains can eventually lead to an overuse injury in the pars interarticularis. The most common location for this to occur is in the lowest vertebra of the spine, which doctors call L5. This vertebra connects the spine to the pelvis. However, a problem with the pars can occur in any lumbar vertebra. It rarely happens in more than one vertebra at a time.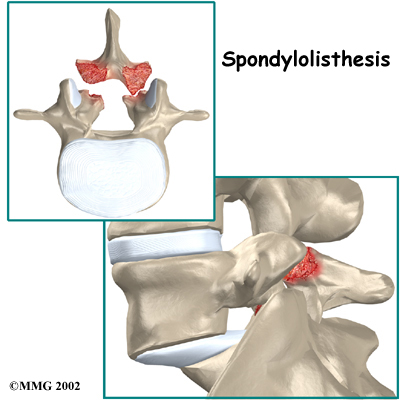
 Individuals may eventually experience pain that radiates down one or both legs. This pain may come from pressure and irritation on the nerves that exit the spinal canal near the fracture. When nerve pressure in the low back causes leg pain, doctors refer it as neurogenic pain.
Individuals may eventually experience pain that radiates down one or both legs. This pain may come from pressure and irritation on the nerves that exit the spinal canal near the fracture. When nerve pressure in the low back causes leg pain, doctors refer it as neurogenic pain.
 Most patients with spondylolysis do not require surgery. When symptoms are not relieved with nonsurgical treatments, however, patients may require surgery. The main types of surgery for spondylolysis include
Most patients with spondylolysis do not require surgery. When symptoms are not relieved with nonsurgical treatments, however, patients may require surgery. The main types of surgery for spondylolysis include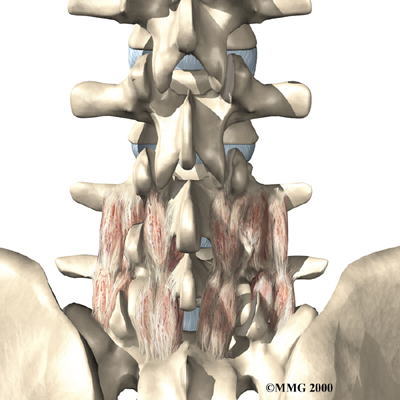 A spinal fusion may be required after a surgeon performs a laminectomy procedure. Fusion is recommended when a spinal segment (a set of vertebrae) has become too loose or unstable.
A spinal fusion may be required after a surgeon performs a laminectomy procedure. Fusion is recommended when a spinal segment (a set of vertebrae) has become too loose or unstable.